Course Info
Updates, Guidance, and Best Practices for Patients with Diabetes
For those of you who provide care to individuals with—or at risk for—diabetes, managing the complex interplay of comorbidities and complications can be challenging. Obesity, a major contributor to the development and progression of diabetes and many of its comorbidities, plays a critical role in patient outcomes and requires targeted strategies for effective management.
With these challenges in mind, Harvard Medical School faculty developed this CME program, Diabetes and Obesity: Complications and Implications, to provide the latest updates, practice recommendations, and evidence-based strategies for optimizing patient care. This program delivers comprehensive education with practical insights to enhance your clinical practice immediately. We will address the following:
- Screening for diabetes and diagnostic criteria for obesity and diabetes
- Clinical approaches to weight management, including lifestyle interventions, pharmacotherapy, and surgery
- Pharmacological management of diabetes, including the latest in insulin and non-insulin therapies and their impact on weight management
- Advances in insulin delivery and glucose monitoring technologies
- Obesity as a comorbidity and its impact on diabetes progression, cardiovascular health, morbidity, and mortality
- Treatment of diabetes-related complications, including dyslipidemia, hypertension, peripheral vascular disease, cardiovascular disease, kidney disease, liver disease, and the diabetic foot
- Care considerations for older adults with diabetes and/or obesity
- Incorporating recent therapeutic advances into your practice
- Challenging patient cases and real-world applications

Education to Optimize Patient Care and Outcomes
Education is focused on optimizing patient care and outcomes and improving skills in the following areas:
- Insulin initiation and intensification: which insulins to choose and why
- Understanding the new insulins, glucose monitors, and pumps
- Treating people with type 2 diabetes who are not achieving therapeutic goals
- Office-based assessment and treatment of comorbidities and complications
- Individualizing multifaceted approaches to lifestyle modification and weight management
- Personalizing nutrition plans and exercise prescriptions
- Cardiovascular risk reduction and care
- Pharmacotherapy for diabetes and obesity: GLP-1 receptor agonists and the spectrum of other options now available
- Optimal management of neuropathies and foot disease
- Managing diabetes in high-risk populations, including pregnant patients and the elderly
- Understanding the evolving concepts and treatments that will soon impact your day-to-day practice
- Communicating with, motivating, and sharing resources with patients
- Recognizing social, racial, sexual, and cultural biases in diabetes care and reviewing strategies for achieving equity and addressing disparities
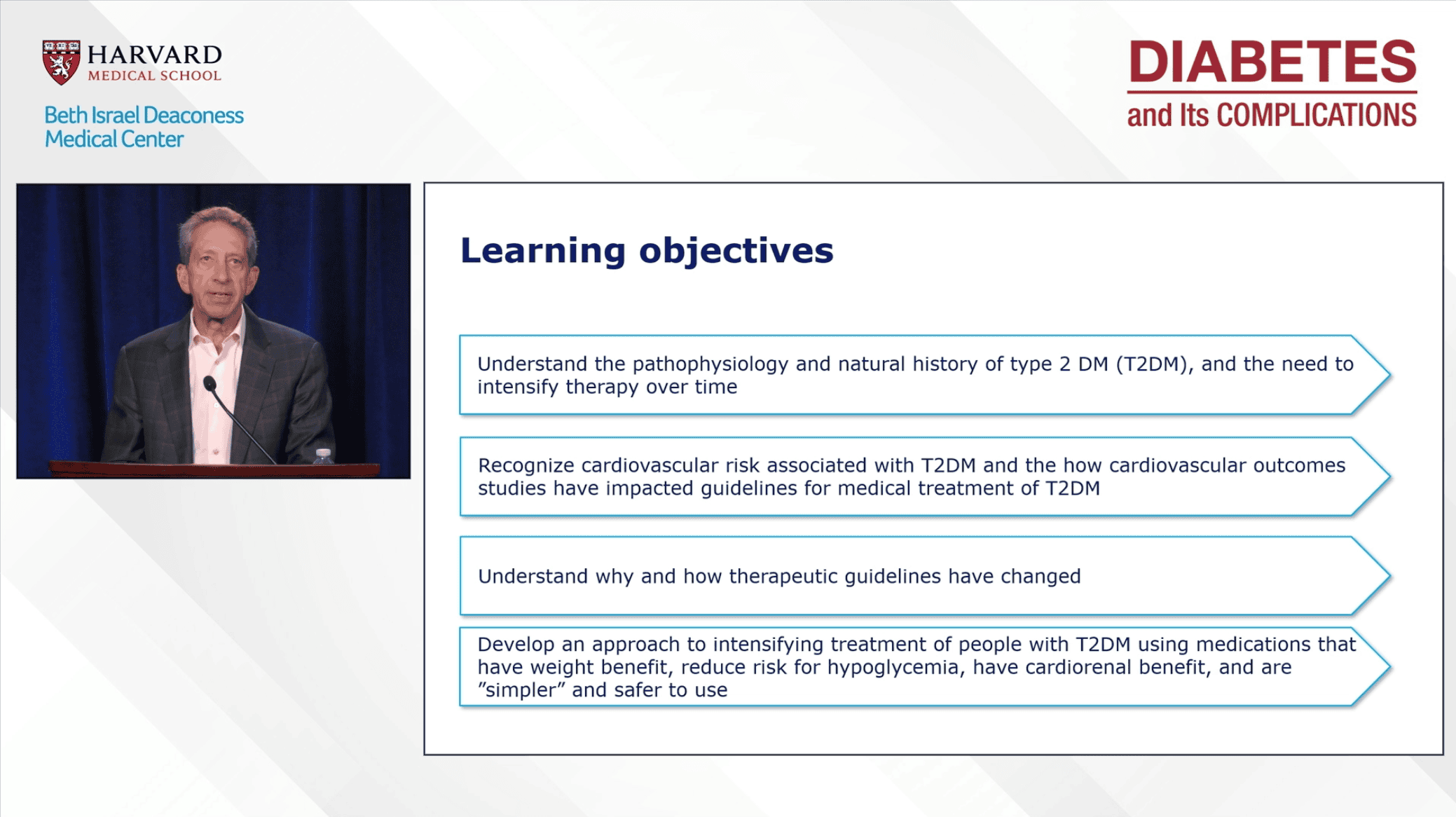
Learning Objectives
At the end of this course, you will be able to:
- Describe the pathophysiology of type 1 and type 2 diabetes, how it is related to the development/progression of key diabetes comorbidities, and how knowledge of pathophysiology drives prevention and treatment.
- Identify ways to improve skills and office-based care systems to optimize lifestyle interventions in the treatment of diabetes, obesity, and related conditions.
- Describe the implications and impact of the latest evidence-based expert treatment guidelines for lifestyle, pharmacologic, and technologic treatments of diabetes and its comorbidities.
- Recognize how the evolving clinical implications of cardiovascular and renal outcomes trials of antidiabetes medications can be effectively applied to the prevention, diagnosis, and treatment of these comorbidities of diabetes.
- Apply the latest preventive, diagnostic, and treatment approaches to the care of the various disease and treatment-related comorbidities of diabetes impacting eyes, nerves, peripheral vascular and foot, liver, bone, and issues with hypoglycemia, and in special populations of people with diabetes such as the elderly, pregnant women, and hospitalized individuals.
- Identify and overcome clinical practice barriers emanating from patients, providers, and practice systems issues.
- Communicate with people with diabetes, families, and health team members in a responsive manner that supports a team approach to the promotion and maintenance of health, as well as prevention and treatment of disease in individuals with diabetes.
Optimized for Remote Learning
What makes this course among the highest-rated Harvard Medical School CME courses:
- Enhanced for distance learning
- Submit questions through the course's online chat; Speakers will either address questions immediately from the podium or reply in the chat
- Participate in online polling feature: Year after year, participants report that the polling feature of this program has advanced their ability to approach complex and challenging cases in their day-to-day practice
- Interactive case-based questions in most presentations
- Session recordings & downloads available for immediate viewing online until February 1, 2026.
Reviews of Our Online Format
“I appreciated attending this meeting from the comfort of my own home. I was able to learn and update my practice while still keeping up with family and work obligations.”
“As a primary care provider, I found that this course did an outstanding job of immersing one into the world of the intensivist.”
“Great speakers, inspiring, smart, and enthusiastic.”
“The virtual option provided an opportunity for me to learn from Harvard Medical School’s best.”
“The instant response to Q&A was impressive and felt like we were connecting in-person.”
“The online platform was excellent and very easy to use.”
